Dementia includes a range of neurological disorders characterised by memory loss and cognitive impairment. Alzheimer’s disease is the most common form of dementia, accounting for 50–70% of cases.1 In 2015 approximately 342,800 Australians were living with dementia, with this number projected to reach 900,000 by 2050.2
Medication management for people with dementia can be a challenge as there are many practitioner-based and patient-based factors that can influence the prescribing or deprescribing of medications. Practitioner-based factors may include incomplete medical histories, lack of time and inadequate guidelines. Patient-based factors include difficulties with comprehension and communication, diminished decision making capacity, and increasing burden of carers.3
Pharmacists have an important role in managing medications for people with dementia. A study conducted in Northern Ireland revealed community pharmacists often encounter community-dwelling people with dementia and have positive attitudes about the management of pain in this patient population. The study identified that further training was needed to improve knowledge.4
Various studies involving pharmacists and seeking to optimise medication management for people with dementia are currently underway across the globe.
In the UK, a focus group study involving people with dementia, informal carers and healthcare practitioners aimed to describe and understand the key challenges with medication management experienced by people with dementia and their carers, and the potential role of community pharmacists. Informal carers said medication management could be challenging due to emotional burden and an implied ‘duty to cope’. They reiterated that ensuring the care recipient was given the correct medication at the right time placed significant emotional burden on the informal carer, which was not always recognised by a healthcare practitioner. Healthcare practitioners said the pharmacist’s role was to provide advice on medications. In contrast, informal carers and people with dementia focused on the practical aspects of the pharmacist’s role, such as home delivery of medication and medication supply. The study concluded there was potential for pharmacists to play an enhanced role for people with dementia and their carers.5
In Sweden, researchers collected data from a randomised controlled clinical trial exploring the effects of a pharmacist intervention as part of a hospital ward team to assess the occurrence of drug-related problems in older adults with dementia and cognitive impairment. The study found clinical pharmacists were identifying at least one drug-related problem in 66% of patients in the intervention group, and ‘unnecessary drug therapy’ was the most common issue identified. Reassuringly, the most common suggested action from the pharmacist was discontinuation of drug therapy. The study also identified that drug-related problems were more common among people taking a higher number of medications and people with an earlier stroke. This study highlighted that medication reviews conducted by clinical pharmacists as part of a healthcare team may play a role in preventing, identifying and solving drug-related problems.6
In Germany, the term ‘Home Medication Review’ (HMR) is taking on a different meaning for people with dementia. The German HMR is a computer-assisted personal interview delegated to specially qualified nurses. Essentially, an HMR is administered by a nursing service where the nurse collects information about medications, medication storage, administration, adherence, adverse drug events, and the daily fluid intake of the patient. Once the HMR system captures the information it compiles a standardised interview report that includes the medication list. The report is forwarded to the patient’s pharmacy and treating general practitioner. The dementia care manager, pharmacist and general practitioner use the information to complete a medication management intervention that involves:
- Pharmaceutical evaluation
- Pharmaceutical recommendations
- Application of recommendations.
This intervention is currently being implemented in a larger trial to evaluate its impact on improving pharmacotherapy and care for people with dementia.7
In Australia, a growing number of groups are dedicated to improving the care and quality of life of people with dementia. A trial of Quality Use of Medicine tools to guide medication management during a Home Medicines Review will begin this month (August).
For more information, visit:
LISA KOULADJIAN O’DONNELL MPS is a practising accredited pharmacist and Postdoctoral Research Associate with the NHMRC Cognitive Decline Partnership Centre, University of Sydney, NSW.
References
- Winblad B, Amouyel P, Andrieu S, et al. Defeating Alzheimer’s disease and vother dementias: a priority for European science and society. Lancet Neurol. 2016;15(5):455–32.
- Australian Institute of Health and Welfare – Dementia. 2016. At: www.aihw.gov.au/dementia.
- Reeve E, Bell JS, Hilmer SN. Barriers to Optimising Prescribing and Deprescribing in older adults with dementia: A narrative review. Current Clinical Pharmacology. 2015;10(3):168–77.
- Barry HE, Parsons C, Passmore AP, et al. Community pharmacists and people with dementia: a cross-sectional survey exploring experiences, attitudes, and knowledge of pain and its management. Int J Geriatr Psychiatry. 2013;28(10):1077–85.
- Maidment ID, Aston L, Moutela T, et al. A qualitative study exploring medication management in people with dementia living in the community and the potential role of the community pharmacist. Health Expect. 2017.
- Pfister B, Jonsson J, Gustafsson M. Drug-related problems and medication reviews among old people with dementia. BMC Pharmacol Toxicol. 2017;18(1):52.
- Fiss T, Thyrian JR, Wucherer D, et al. Medication management for people with dementia in primary care: description of implementation in the DelpHi study. BMC Geriatr. 2013;13:121.












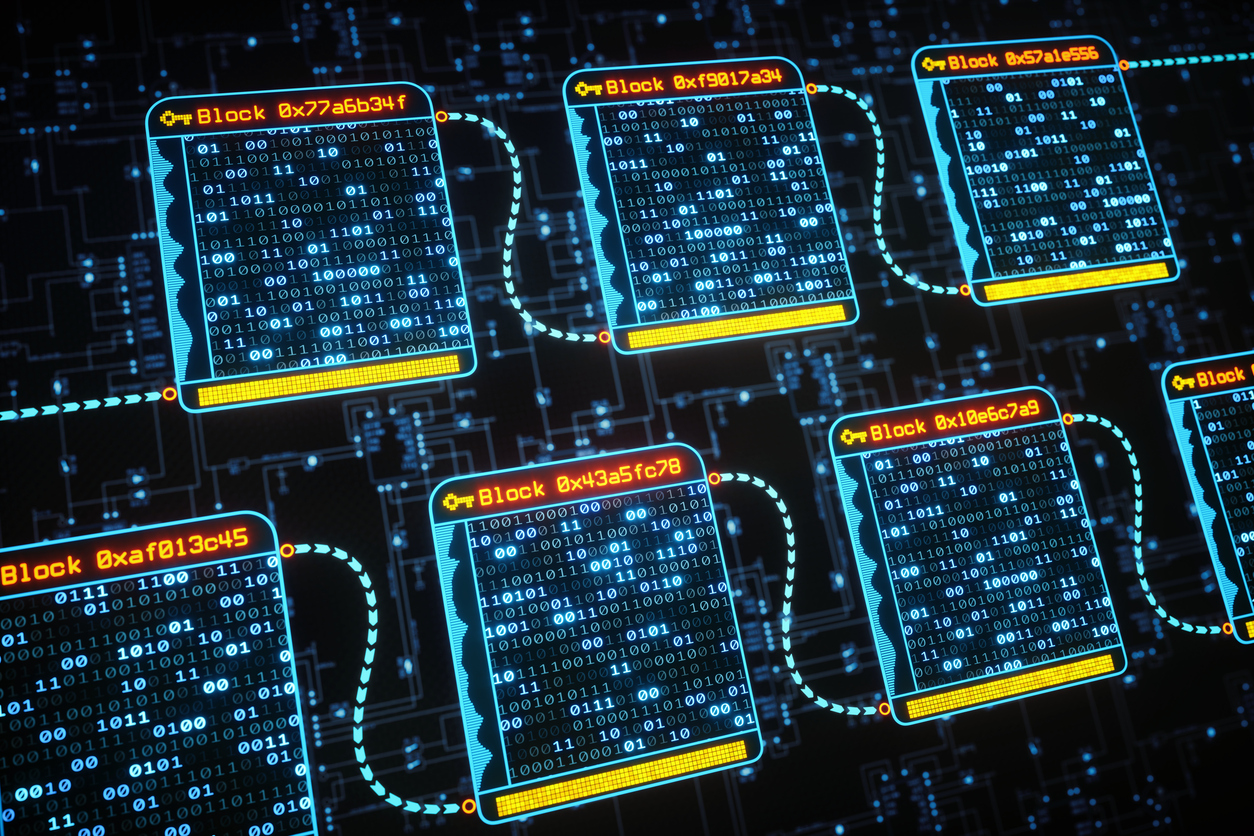

 PSA Chief Operating Officer Deb Bowden, Senator Zed Seselja and PSA National President Dr Shane Jackson.[/caption]
PSA Chief Operating Officer Deb Bowden, Senator Zed Seselja and PSA National President Dr Shane Jackson.[/caption]





 [post_title] => New Pharmacy House opens
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => new-pharmacy-house-opens
[to_ping] =>
[pinged] =>
[post_modified] => 2018-04-05 12:33:52
[post_modified_gmt] => 2018-04-05 02:33:52
[post_content_filtered] =>
[post_parent] => 0
[guid] => http://psa.studionerve.com/?p=1231
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => New Pharmacy House opens
[title] => New Pharmacy House opens
[href] => http://psa.studionerve.com/new-pharmacy-house-opens/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 1239
)
[post_title] => New Pharmacy House opens
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => new-pharmacy-house-opens
[to_ping] =>
[pinged] =>
[post_modified] => 2018-04-05 12:33:52
[post_modified_gmt] => 2018-04-05 02:33:52
[post_content_filtered] =>
[post_parent] => 0
[guid] => http://psa.studionerve.com/?p=1231
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => New Pharmacy House opens
[title] => New Pharmacy House opens
[href] => http://psa.studionerve.com/new-pharmacy-house-opens/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 1239
)